The ability to digest and break down food requires harmonization across dozens of different types of cells and many tissues.

Heading this process is the gut’s nerve cell network, the enteric nervous system, which winds throughout the body’s intestinal walls and functions nearly independently from the brain, even earning the nickname “the second brain.” And much like the brain, this system is comprised of two types of nervous cells: neurons and glial cells.
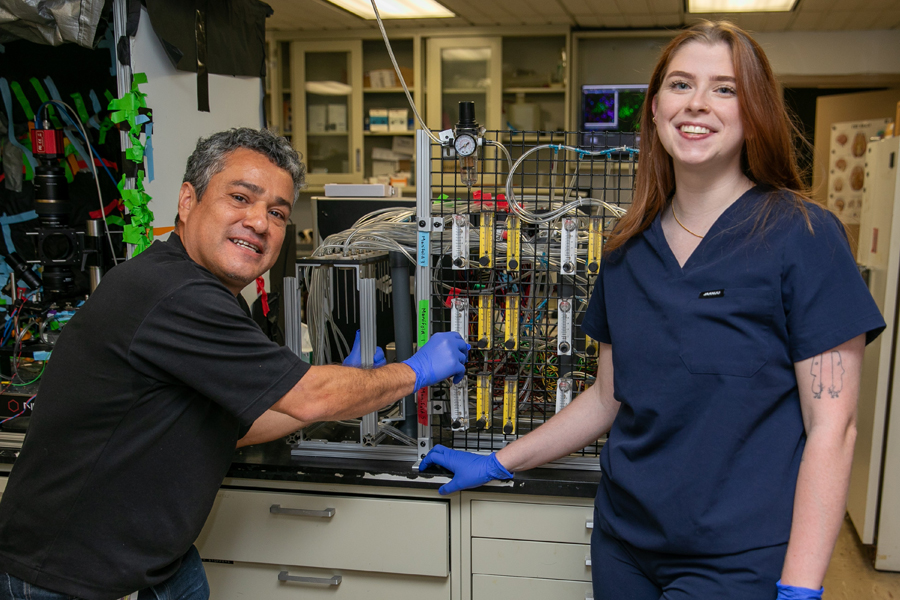
However, much remains unknown about how these cells contribute to many gastrointestinal and neurological diseases. That’s where neurobiologist Vladimir Grubisic, M.D., Ph.D., assistant professor of biomedical sciences at the College of Osteopathic Medicine (NYITCOM), comes in.
Assisted by research associate Anthony Pellicano, M.S., and two dozen student researchers in his busy laboratory, Grubisic aims to solve these microscopic mysteries and deliver findings that could pave the way for new treatments benefiting patients with inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), colon cancer, autoimmune disease, metabolic conditions, and neuropsychiatric disorders.
New York Tech News sat down with Grubisic to learn more about his team’s research.
What are glial cells?
The term glia comes from the ancient Greek word for “glue,” reflecting the beliefs of neuroscientists from the 19th and early 20th centuries, who theorized that these cells functioned solely as a connective tissue that simply held the neurons together. Now we know that glial cells do far more than provide structural and passive support for the neurons—they actively regulate many important processes, including learning, memory, breathing, and sleep.
There are many types of glia in the central nervous system, such as those in the brain and spinal cord, as well as in the peripheral nervous system. Meanwhile, enteric glial cells reside in the gastrointestinal (GI) system, embedded in all the layers of the digestive tube, where they actively contribute to the regulation of gut neural reflexes, such as motility and secretion.
How are these cells potentially linked to gastrointestinal disease?
Under healthy conditions, enteric glia act as cellular hubs, interacting with the gut’s immune cells, epithelial cells that form the inner lining of the intestinal barrier, and nerves. As such, they play a key role in maintaining gastrointestinal tract function and measuring immune responses.
The intestinal barrier is designed to be selectively permeable, allowing for nutrient absorption while keeping out harmful substances. However, enteric glia can also promote inflammation and dysfunction by increasing barrier permeability. Under these conditions, known as “leaky gut,” toxins and microorganisms may pass through the intestinal barrier, causing local inflammation within the bowel wall that can further exacerbate barrier penetrability and increase the risk of noxious compounds leaking into the bloodstream. The condition is implicated in gastrointestinal diseases like Crohn’s disease (a type of IBD), as well as various systemic disorders, such as multiple sclerosis, type I and II diabetes, obesity and metabolic syndrome, autism, anxiety, depression, Alzheimer’s disease, and Parkinson’s disease, to name a few. We are investigating the specific cell and molecular mechanisms that regulate the intestinal epithelial barrier in health and disease; this work has the potential to uncover new avenues for specific leaky gut treatments.
How are students involved in this research?
Students’ roles are tailored based on their educational background and theoretical knowledge, prior wet lab experiences, and their own inclinations, motivations, or restrictions. Usually, everyone gets to learn the dissection of preserved animal intestinal tissues, along with basic immunostaining, fluorescent microscope imaging, and image analysis. The other responsibilities may involve working with live specimens, such as in vivo assays of gut motility or gut permeability; experiments on live intestinal tissues, including gut smooth muscle contractility, in situ calcium imaging, and tissue electrophysiology; and in vitro experiments on cultured cells isolated and derived from animal tissues.
Soon, we will start receiving intestinal biospecimens from human patients through our collaborators at Columbia University. Given sufficient commitment to time and motivation, students can also work with the world-class super-resolution fluorescent microscopy and spatial transcriptomics located in the Biomedical Research, Innovation, and Imaging Center. We usually have between four and seven students working in the wet lab at a time.
Which students are currently working in your laboratory?
Currently, this includes NYITCOM students Sayida Afghani, Jake Borenkoff, Katherine Gilpin, Shauna Harney, Juliet Insinga, Austin Irwin, Madison Kalter (co-supervised with NYITCOM faculty Julia Molnar, Ph.D., and Brian Beatty, Ph.D.), Bohdan Klotska, Bryan Koflanovich, Alexander Malayev (co-supervised with NYITCOM faculty Olga Savinova, Ph.D.), Anna Mienko, Juliana Niyazov, Andrew Novello, Enaea Sahloul, Szymon Samborski, Rupinder Singh, Abdul Wahid, Abigail Wolf, and Nicholaos Xenakis. New York Tech undergraduates currently include Maryam Iqbal, Alexander Kaminer, Namira Hossain, Vidisha Maharana, and Christina Wilson.
Is your team involved in any other studies?
We’re actively researching the role of enteric glia and leaky gut in neurodevelopmental disorders, such as autism, and neurodegenerative disorders, such as Alzheimer’s disease. Our efforts in these areas are helped through collaborations with NYITCOM faculty neuroscientists, including Gonzalo Otazu, Ph.D., Raddy L. Ramos, Ph.D., and Randy Stout, Ph.D. We also study gut dysfunction in heart failure through a collaboration with fellow NYITCOM faculty researchers Kaie Ojamaa, Ph.D., and Olga Savinova, Ph.D.
In addition, we have been working with New York Tech faculty investigators Michael Hadjiargyrou, Ph.D., and Henry Ruiz, Ph.D., in the College of Arts and Sciences. We recently started translational research investigating small molecule modulators designed and synthesized by our collaborators at SUNY at Buffalo. Very recently, we also began planning collaborative projects with Karrer Alghazali, Ph.D., from the College of Engineering and Computing Sciences.
This interview has been edited and condensed.
More News

Study: VR Helps Children With Autism Participate in Exercise and Sports
A new study by researchers from the School of Health Professions and College of Osteopathic Medicine demonstrates how virtual reality (VR) can help children with autism spectrum disorder participate in exercise.
Driven by ‘Why’
Third-year medical student Kassandra Sturm leads the charge on a new study helping to uncover the neurological source affecting the sense of smell in autism spectrum disorder.
Technology Partnership Helps Children With Disfluencies
Former NBA star Michael Kidd-Gilchrist has partnered with the College of Engineering and Computing Sciences’ ETIC to develop a prototype of a technology platform that he hopes will help children who stutter.

Engineering a Cancer Treatment Game Changer
A groundbreaking project co-led by the College of Engineering and Computing Sciences’ Steven Zanganeh, Ph.D., provides the world’s first functional, drug-testable, 3-D-printed human colon model.

Edward Guiliano Global Fellows: Culture Across Continents
Under the Edward Guiliano Global Fellowship program, seven students traveled the globe, broadening their perspectives and working on transformational research projects.

Faculty Secure Federal Research Grants
The National Institutes of Health and the National Science Foundation recently awarded funding to multiple faculty-led research projects, totaling more than $2.8 million collectively.