Using AI to Detect ECG Abnormalities
The growing use of artificial intelligence (AI) for medical applications is creating new tools for physicians to provide better patient care and improve health outcomes. Two recent student-led research projects have uncovered potential new uses of AI modeling techniques for heart health, increasing the efficiency and accuracy of cardiac diagnoses.
In a collaboration between the College of Osteopathic Medicine (NYITCOM) and the College of Engineering and Computing Sciences Entrepreneurship and Technology Innovation Center (ETIC), students and faculty worked on complementary research projects to detect electrocardiogram (ECG) abnormalities using AI models. The two groups approached the research from different angles—one from a clinical perspective and the other from a computer engineering perspective.
Thanks to the College of Engineering and Computing Sciences’ collaborative agreement with Catholic Health on Long Island, the two research teams obtained a robust set of anonymized ECG data. The two individual New York Tech research teams worked together to clean and normalize the data to create a reliable dataset of ECG results that they could use for analysis, prediction, and decision-making. The two teams then used the dataset to train and test multiple AI models to identify the algorithms that produced the most accurate and consistent predictions.

“The AI model could produce output that establishes results as abnormal, and then a doctor can go back and look at the result again if the AI model is showing something different than what they’re interpreting as medical professionals,” says Michael Nizich, Ph.D., director of the ETIC. “We’ll always need the professionally trained doctor, and this model can give the medical professional one more tool to use through the results stemming from these students’ efforts.”
The two research teams shared the same goal—to develop an AI model to help clinicians determine whether ECG results are normal, abnormal, or borderline—but they approached the task with different priorities and evaluation standards. Their faculty supervisors were not surprised that the two research groups presented different ideas about which AI model worked best within the ECG dataset they used for the study.
“The ETIC-led study focused more on the technical and methodological aspects—analyzing the data, optimizing algorithms, and explaining the engineering principles behind the models. They prioritized finding the model with the highest test-set accuracy,” says Milan Toma, Ph.D., assistant professor of clinical sciences at NYITCOM. “In contrast, the NYITCOM-led study focused on whether high accuracy was also credible and clinically reliable. The clinical approach prioritized the practical application of the AI model in diagnosing ECG abnormalities, emphasizing clinical relevance, patient outcomes, and interpretability. Medical experts require this kind of evidence to trust that a model will perform well in real-world clinical situations, even if its initial accuracy is slightly lower than other models that don’t demonstrate such reliability.”

Coming to Conclusions on AI Models
The two New York Tech research teams, with researchers from Catholic Health, set out to identify AI models that would help physicians interpret ECG results with high accuracy and consistency. The Catholic Health ECG dataset included clinical features and key ECG measurements but did not include time-series data (the continuous recording of ECG signals over time). Using an AI model, the teams explain, physicians can address the challenge faced by healthcare facilities with limited resources (for example, those without access to time-series data) when categorizing ECG results as normal, abnormal, or borderline. A reliable AI tool could potentially extend diagnostic support to a broader range of clinical environments and, in turn, improve patient care in those settings.
In the paper “Electrocardiogram Abnormality Detection Using Machine Learning on Summary Data and Biometric Features,” lead author Kennette James Basco (B.S. ’23, M.S. ’24) and other ETIC researchers trained multiple AI models and concluded that extremely randomized trees performed better than the other machine learning algorithms they trained, with overall higher recall and accuracy rates than other algorithms.
In contrast, the NYITCOM research group’s paper, “Clinical Applicability of Machine Learning Models for Binary and Multi-Class Electrocardiogram Classification,” concluded that the deep learning algorithm called convolutional neural networks (CNN) achieved the best balance between generalization and performance for classifying ECG signals as normal, abnormal, or borderline.
Daniel Nasef, a second-year NYITCOM student and lead author of that paper, emphasizes the importance of the generalizability of research results. In other words, a clinician must be able to trust that the AI model’s prediction would be accurate for any patient at any hospital.
“The model isn’t helpful if it is not generalizable,” Nasef says. “Correctly predicting disease in patients in a given dataset does not necessarily mean it would be applicable to outside patients or data.”

The Benefits of Interdisciplinary Research
Even though the two groups arrived at different conclusions about which AI model might be best for helping physicians interpret ECG results, these kinds of research studies are crucial to improving medical care and patient outcomes.
“This difference highlights why collaboration between engineering and medical experts is so important: Engineering teams often focus on maximizing technical performance, while medical teams ensure that the results are meaningful and safe for patient care,” Toma says. “Only by combining both perspectives can we develop AI tools that are both high-performing and truly trustworthy in clinical practice.”
“This collaboration exemplifies the transformative power of interdisciplinary research and student-driven innovation,” says Babak Beheshti, Ph.D., dean of the College of Engineering and Computing Sciences. “It reflects our commitment to advancing healthcare through the combined strengths of engineering, medicine, and data science. It’s a powerful example of how real-world partnerships can lead to meaningful research and impactful publications.”

The interdisciplinary collaboration was eye-opening for the students, who learned to view the task and the potential solution from multiple perspectives.
“When I’m given a dataset, I see just numbers. When studying machine learning, we train a model to detect patterns in those numbers,” says Basco, who earned both of his degrees in computer science. “But ECG data are about physical health and making diagnoses, so you have to put more scrutiny on the prediction of those models. I had to improve the model in a way that’s not compromising the health of the patient.”
After collaborating with clinical researchers, Basco wants to pursue a computer science career in a medical setting.
“I’m applying for jobs at hospitals now rather than at tech companies because helping individuals with their health is rewarding,” Basco says. “Doing this research opened up more career avenues for me. I got to put my name out there as a researcher and contribute to the science.”
Nasef is eager to continue conducting research as a medical student and during his residency in the future.
“Dr. Toma entrusts you with a lot of responsibility, which is frightening but also empowering,” Nasef says. “I look at each research project as an opportunity to grow and get better at using machine learning in a clinical setting.”
Nizich emphasizes that these kinds of interdisciplinary research collaborations benefit not only the students individually but also the field of medical AI research as a whole.
“Advanced AI research can cost millions of dollars and become cost prohibitive,” Nizich says. “In a higher-ed research environment, we have students who want to work on real-world research projects. We have the ability to make a new discovery and publish it for the world to use. The interdisciplinary work of these projects is unique, and it builds our students’ résumés and helps them in the job market.”
By Ashley Festa
More News
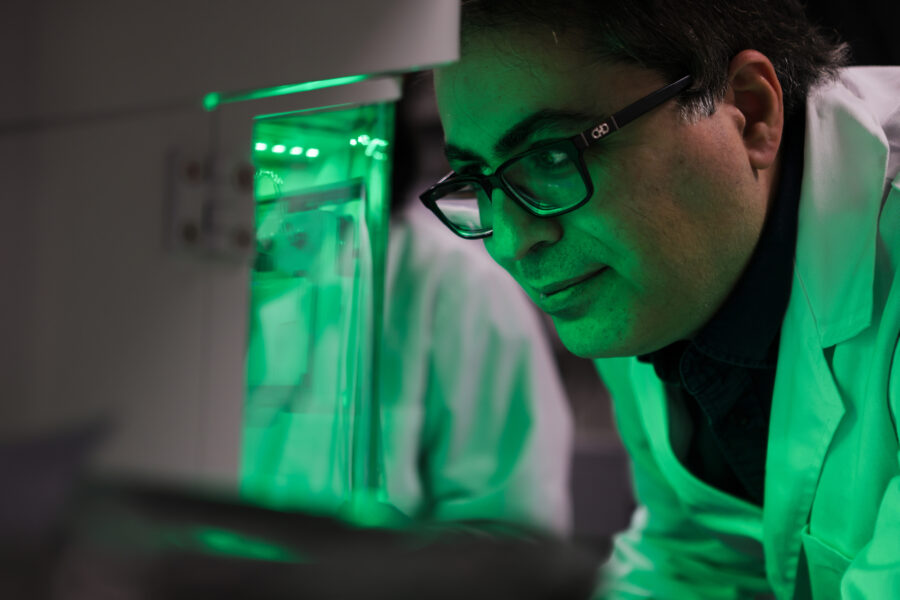
Realistic 3-D Colon Model Shifts Paradigm for Drug Development
Assistant Professor Steven Zanganeh, Ph.D., is striving to further improve the model he developed to open the door to drug development for cancer and other conditions.

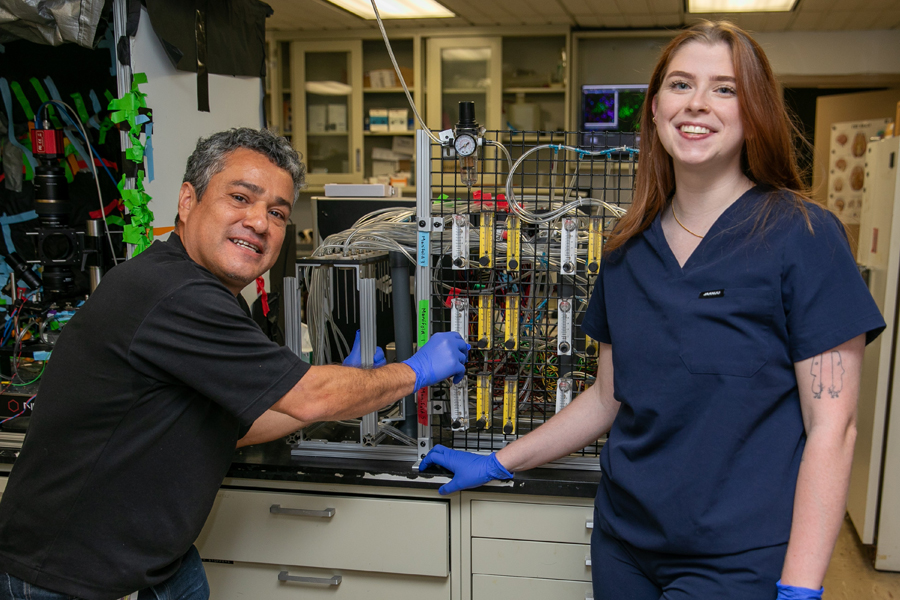
Understanding the Human Machine
Biology student Justin Tin seeks to understand what’s running “under the hood” in the human body so he can someday help prevent patients from suffering physiological changes.

Study: VR Helps Children With Autism Participate in Exercise and Sports
A new study by researchers from the School of Health Professions and College of Osteopathic Medicine demonstrates how virtual reality (VR) can help children with autism spectrum disorder participate in exercise.
Driven by ‘Why’
Third-year medical student Kassandra Sturm leads the charge on a new study helping to uncover the neurological source affecting the sense of smell in autism spectrum disorder.
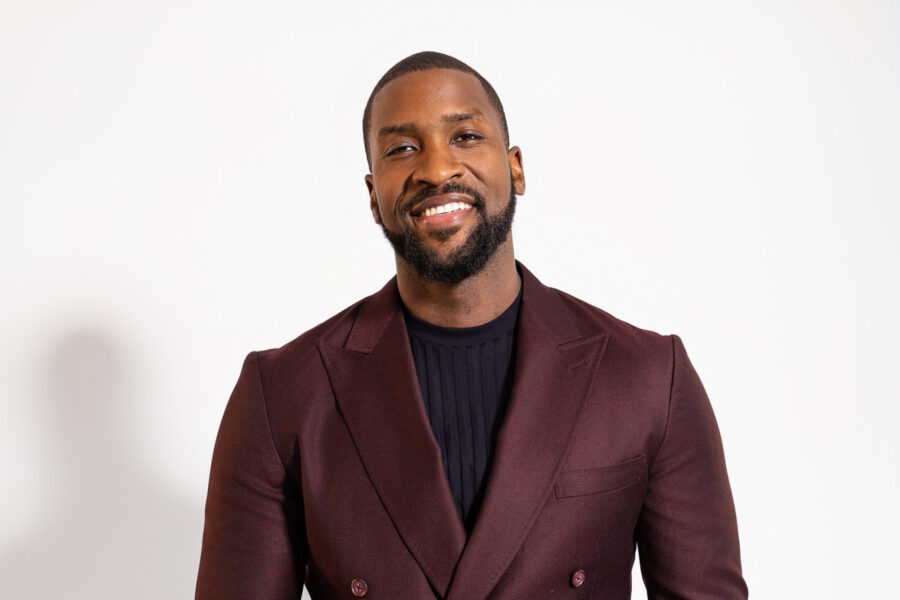
Technology Partnership Helps Children With Disfluencies
Former NBA star Michael Kidd-Gilchrist has partnered with the College of Engineering and Computing Sciences’ ETIC to develop a prototype of a technology platform that he hopes will help children who stutter.

Engineering a Cancer Treatment Game Changer
A groundbreaking project co-led by the College of Engineering and Computing Sciences’ Steven Zanganeh, Ph.D., provides the world’s first functional, drug-testable, 3-D-printed human colon model.