News
Active Research: Going Head-to-Head Against Concussions
July 19, 2019
TOP PHOTO: Using digital mouthguards. NYIT men’s lacrosse student-athletes took part in a study to measure impacts during play.
Experts at NYIT’s Center for Sports Medicine are leading the charge on concussion care and research.
According to claims data from Blue Cross Blue Shield, concussion diagnoses increased 43 percent between 2010 and 2015. Diagnoses of children and teens increased by 71 percent (likely fueled by the student-athlete population). Not only do these young people suffer more concussions, they experience the effects longer than adults.
Researchers at NYIT College of Osteopathic Medicine and NYIT School of Health Professions are fighting back. At the Center for Sports Medicine, medical professionals are taking a leading role in providing comprehensive care for concussion patients, including student-athletes from NYIT, Long Island University’s Post campus, and nearby Long Island high schools.
Through research, we want to offer the best quality treatment for patients suffering from head injuries.
Hallie Zwibel
“Through research, we want to offer the best quality treatment for patients suffering from head injuries,” says Center for Sports Medicine Director Hallie Zwibel, M.P.H. (D.O. ’11). “Student-athletes—and all of our patients—benefit from medical personnel, technology, and resources that most other concussion centers simply don’t have.” That includes an interdisciplinary approach to care from a team of providers— including physical therapists, occupational therapists, psychologists, neurologists, and physicians with special training in musculoskeletal medicine—all in one place.
“Student-athletes have their whole lives ahead of them,” says Eric Greenberg, PT, D.P.T., SCS, CSCS, assistant professor of Physical Therapy and a member of the Center for Sports Medicine team. “It’s our priority, as rehabilitation specialists, to ensure they return safely. That decision is made by medical personnel, the athlete, and the coaching staff and depends entirely on specific circumstances.”
While most concussion research has focused on football, recent studies at NYIT have looked at what happens to athletes who suffer subconcussive hits, which Zwibel defines as “impacts that don’t result in concussion but might happen repeatedly during a game.”

Hallie Zwibel assesses the balance of a patient.

Eric Greenberg provides physical therapy services to a student-athlete.
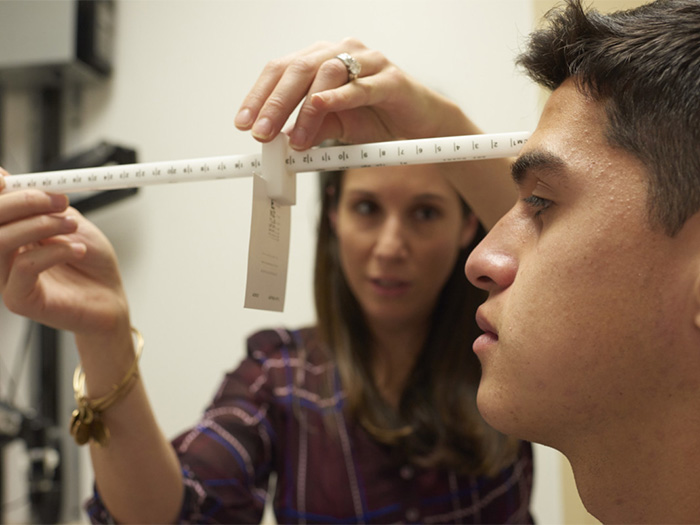
Christina Finn performs a vision test for concussion symptoms.
In spring 2018, the Center for Sports Medicine partnered with the NYIT men’s lacrosse team to understand the effect repeated “checks” during play have on athletes. Ten student-athletes wore mouthguards with digital sensors that measured impacts throughout the season. The results were enlightening. One athlete sustained more than 1,700 hits, many measuring over 80gs of force, the equivalent of being in a 40-mile-per-hour car accident while wearing a seat belt.
Remarkably, the student-athletes did not detect any noticeable difference in their memory or reaction time, but cognitive testing revealed subtle declines in verbal and visual memory and cognitive reactions. “It’s these subtle differences that could cause significant problems long term,” says Zwibel.

Bhavesh Joshi, D.O., and NYITCOM-Arkansas medical students Colton Eubanks (left) and Lucas Eeftink (right) treat athletes during games and practices.
In fall 2018, researchers continued the study and asked members of the NYIT women’s soccer team to wear sensors to measure impacts. They also tested salivary biomarkers. “Studies show that you can examine these different markers not only to diagnose a concussion, but also to see who’s at greater risk for a prolonged symptomology,” says Zwibel, who adds the information could lead to real breakthroughs. “A lot of people play football, but not everyone is getting CTE [chronic traumatic encephalopathy], right? We’re trying to see what is predisposing people to long-term consequences.”
As an occupational therapist in the School of Health Professions, Assistant Professor Christina Finn, Ed.D., is also focused on combating concussions. Working in the NYIT Center for Sports Medicine, she does vision screenings for patients, develops treatment plans, and is involved in concussion education programs for coaches and parents. For her dissertation, Finn created a training program for faculty members on concussion and its impact on academic performance.
SIDELINE SUPPORT
At NYITCOM-Arkansas, Sports Medicine Specialist Bhavesh Joshi, D.O., assistant professor of Clinical Medicine, ensures his students do more than stand on the sidelines of sports injury research and medicine. He and a team of students travel with the Division I A-State football team to provide medical assistance. “They are able to apply their history taking, physical exam skills, and osteopathic manipulation in an integrated real-world experience,” he says. “I love having students shadow me to see how wide and diversified the field of medicine can be!”
Now at NYIT, she’s employing smart technology in her research by using a Fitbit and smartphone app to help patients track concussion symptoms. “When a student feels symptoms, such as headache or nausea or dizziness, they indicate that on the app and log what they’re doing in terms of activity,” Finn explains. She then compares that information with data from the Fitbit to see if there was an increased heart rate or other physiological response. “By keeping track of symptoms, we can help patients determine what activities or environments provoke those symptoms so they are better able to manage them,” says Finn.
Center for Sports Medicine practitioners also use osteopathic manipulative medicine (OMM)—a tenet of osteopathic medical care—to treat concussion patients and study its impact on recovery.
Sheldon Yao (D.O. ’02), associate professor and chair of the Department of Osteopathic Manipulative Medicine, is leading an ongoing study to compare concussion patients who receive OMM with those who only receive counseling. “Any athlete that has a concussion needs to be cleared by our physicians,” says Yao. They also can participate in a research study investigating the effects of OMM on sports concussion injuries. So far, 32 people have signed up for the study.
With many concussion injuries, the person suffers something similar to whiplash—the head gets knocked around and the muscles spasm. “That contributes to their pain, headache, and other concussion symptoms,” Yao explains. Already, he says, the study has demonstrated that the group treated with OMM had significant improvements in terms of symptom severity and number of symptoms compared with patients who did not receive OMM. Yao recently submitted the research for publication. “The results are important because there are very few treatment options for concussion, and OMM can potentially reduce concussion symptoms to help the athletes recover quicker,” he says.
Adds Zwibel: “We believe that if we can manipulate part of the body to put it into proper alignment, it helps the body heal itself.”
SIDELINE SUPPORT
At NYITCOM-Arkansas, Sports Medicine Specialist Bhavesh Joshi, D.O., assistant professor of Clinical Medicine, ensures his students do more than stand on the sidelines of sports injury research and medicine. He and a team of students travel with the Division I A-State football team to provide medical assistance. “They are able to apply their history taking, physical exam skills, and osteopathic manipulation in an integrated real-world experience,” he says. “I love having students shadow me to see how wide and diversified the field of medicine can be!”
By Renee Levy




